Naso-Gastric (NG) Feeding Tubes
Naso Gastric Tube feeding can sound frightening to brand new parents who have never experienced it before. This article is written from personal experience to reassure anxious parents and arm you with all the facts. There are further resources listed at the end that may be useful to print out and give to relatives who will have lots of questions.
What is Nasogastric Tube Feeding?
In the simplest of terms, NG Tube feeding describes the insertion of a tube up the nose and down into the stomach. It is the method used to feed premature or poorly babies who are unable to take milk from either the breast or the bottle, or who need a little extra help topping up their tiny tummies if they tire before they are full. It allows your baby to get the nutrition they need to grow and develop and therefore it is a good thing and not a cause for alarm, which I appreciate is easy to say and perhaps hard to believe! NG feeding is also used for older children who are unable to eat efficiently.
How does NG Tube feeding work?
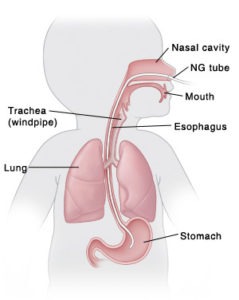
The NG tube passes through the baby’s nose and down the back of their throat into their stomach. Ears, nose and throat are all connected and therefore no surgical intervention is required to set up a naso gastric tube. The tube passes down the oesophagus (the tube we use to swallow) and directly into the stomach. The oesophagus and the trachea (the tube we use to breathe) are completely separate so a correctly inserted NG tube is absolutely not a choking risk.
This simple diagram from St Luke’s Health System demonstrates this clearly.
How do they put a NG feeding tube in?
It is essential that this is done by an experienced medical professional or by someone who has undergone the correct training. There are various things that can go wrong if the tube is inserted incorrectly, for the sake of this article we are working with the assumption that you are not attempting this at home on your own without help!
Firstly the medical staff will measure the distance from the tip of the nose down to the tummy so they know how long to make the tube.
The tube is fed up the baby’s nostril and down into the stomach and whilst it is not a pleasant procedure to watch it is quick and painless for the baby. The nasal route is preferred as it is more secure, although it is possible that they will choose to go in through the mouth in some children (known as Orogastric Tube Feeding).
Once the tube is in place it is secured with surgical tape next to the nose and trimmed to allow it to trail loose. The tube is then sealed off ready for use with a valve.
How does NG feeding work?
When the baby is ready to be fed a nurse will attach a syringe to the end of the tube via the special valve. The breast milk or formula is poured into the syringe and sometimes a tiny amount of pressure is applied with the plunger to get the liquid flowing. The syringe is then held up to allow gravity to do its thing! It is important that it isn’t held too high or too low as this affects how fast the liquid flows in to the baby’s stomach. Typically it is 10 inches or less but the medical staff will know the correct height and teach it to parents and carers in the neonatal unit.
The lovely thing about NG feeding is it allows both parents to feed the baby and also you know exactly how much they have had – unlike breastfeeding which always felt like a bit of a guessing game depending on how tired and productive I was!
Does NG feeding hurt my baby?
No. It is painless and causes no distress to the baby. When they change the tube they will also have to remove and change the surgical tape. This was the only bit my son really objected to but they gave him a tiny bit of sugar solution first which helped a lot.
Does NG feeding damage my baby’s throat?
Again no. The tube is very small so it doesn’t fill the oesophagus and it is very soft so causes no scratching or damage to the back of the throat and top of the stomach.
Will my baby choke on a nasogastric feed?
Another no. As per the diagram above, the oesophagus is completely separate to the trachea (the tube that we breathe through that leads into the lungs) Of course there is risk involved if the tube is placed incorrectly but the staff are very carefully trained to avoid this happening.
How do they know when NG feeding is no longer necessary?
There are lots of factors which the medical staff will look for. In the case of premature babies with no suck reflex they will start to demonstrate new behaviours as they feed which may include sticking out their tongue or sucking at their fingers. What the doctors are looking for is a steady weight gain and periods of alertness. Removing the tube is quick and painless and causes no lasting damage.
Will they need to change the NG tube?
Yes, sometimes they do need to change the tube. This is often just to give one nostril a rest so they are likely to change sides if the tube is in for more than a couple of days. Again, this is normal and nothing to be alarmed by.
Will my baby try to pull out the NG tube?
Another yes. With NG tube feeding the most common issue is that the baby will pull the tube out by wriggling tiny fingers between their face and the tube and giving a good old yank. It’s not a sign of distress or discomfort, in fact pushing things away from their face is a normal, healthy reflex, just like gripping your finger or turning their face towards a gentle touch on their cheek. Don’t panic the nurses will be on hand to replace it. You can minimise this happening by covering your baby’s hands with scratch mitts for older more active babies and children, ScratchSleeves are an effective solution.
Finn’s Story
This post is written from personal experience of NG feeding. This is my son’s experience and I hope will be relatable and reassuring!
Finn was born 6 and a half weeks early and spent the first two weeks of his life in the Special Care Baby Unit at Winchester’s Royal Hampshire County Hospital. There are all sorts of reasons that babies may require a NG tube but in his case it was because he had no suck reflex as this doesn’t develop until 36 weeks gestation. As he was born by emergency C-section I wasn’t there to witness all the tubes and cannulas being inserted as I was in the operating theatre, however my husband went down with him in his incubator and sat on a stool whilst the nurses swept in. He describes it as very scary as we had no previous experience to go by and having a premature baby was not something we had ever imagined happening. By the time the nurse took a polaroid of him to bring up to me in recovery he was all kitted out with a dazzling array of tubes and monitors, including the nasogastric tube.
For the first couple of days there was very little we could do as parents for him. Because he was so tiny and fragile we could only hold him for a couple of minutes at a time, and we needed one of the nurses to detach him from all the monitors and pass him to us. As a mum I found this quite distressing and a far cry from all the images we have of being passed our newborns to cuddle immediately against our breast ready to start feeding. However, the staff at RHCH were fantastic and told us that one of the first things we would be able to do was feed him via the tube.
Having watched the nurses do it several times we were both terrified to try it, which apparently is absolutely normal. Luckily for me my own mother was a paediatric nurse at St Thomas’ Hospital in London for years and she treated NG feeding no differently to giving a bottle to my nephew and niece when they had been born a few years earlier. We learned how to hold the syringe, how to lower it to stop the flow to burp him midway (a skill which I never quite mastered but that my husband was irritatingly good at!), how to remove the syringe and recap the valve and how to tell when he was full (the liquid basically just stops flowing)
After a few days it felt completely normal and we were confident and efficient (and rather proud of ourselves too!). Of course, any new parent knows that the moment you have mastered something your baby ups the ante by developing a new habit or finding a way to outsmart your progress. Finn’s first trick was to pull out his feeding tube. The first time he did this I was horrified but the nurses reassured me that it is a natural reflex and they calmly reinserted it and carried on as though nothing had happened. Panic over. I soon learned that this was going to be a daily occurrence and to take it in my stride alongside meconium poo (which was like tar!) and being weed at with alarmingly good aim the moment I undid a nappy!
After a week of NG tube feeding, Finn started to suck his fingers during a feed (one of the signs I mentioned above) and so I started the slow introduction to breast feeding. He remained on a Nasogastric tube for another few days so they could be sure he was getting enough to eat but the wet nappies and increasing periods of alertness soon meant the tube could come out with the option to reinsert should his weight start to drop. Throughout the time he had the NG tube in I was encouraged to express and he was given this milk topped up with formula. If you are not wanting to breastfeed or milk is slow to come in be reassured that this step is not necessary, this was just my personal choice.
Once the NG feeding tube was out they removed the apnoea monitor too (an alarm which goes off if they don’t take regular breaths, again because he was so early his lungs were not as strong as a term baby). Funnily enough when this happened and they moved him to special care from intensive care I actually found it far more stressful – tube feeding had been extremely reassuring in the end and I didn’t want it to stop! Of course, the day came when he was discharged and we were allowed to take him home. Which was both thrilling and terrifying! He had no lasting damage from the tube and is now a strapping 11-year-old who is rugby obsessed and as tall as me.
One thing I do wish we had had during his time in intensive care was a way to prevent him from pulling out the NG tube. ScratchSleeves have been making an effective solution to eczema scratching for 14 years and have branched out over the years to encompass other areas, including burns, post-operative care and even has an adult range for the dementia market. So ScratchSleeves had a batch of prem size ScratchSleeves made up specifically for NG feeding as the silk mittens make it impossible for little fingers to pull out the tube. We donated them to RHCH as a thank you for all their incredible efforts and they have proven to be a great success.
Further reading
These articles are all great at explaining the process of Nasogastric tube feeding and make for helpful reading, especially for relatives who may also not have come across it before.
- This article from Bliss gives a simple and concise guide to NG feeding which may be helpful for older siblings to read or listen to Tube feeding | Bliss
- This leaflet from the National Health Service provides all you need to know about neonatal nasogastric tubes and newborns LN003881.pdf (leedsth.nhs.uk)
- This video from the Global Health Media Project shows NG tube feeding in action and is calm and reassuring Feeding with a Nasogastric Tube – Small Baby Series – YouTube


Quick buy





